The Role of Aerobic and Anaerobic Respiration and Cerebral Misery Perfusion in Chronic Fatigue Syndrome (Myalgic Encephalomyelitis)
Let’s start by going back to high school biology class, starting with respiration.
You take a breath in and your lungs fill with oxygen.
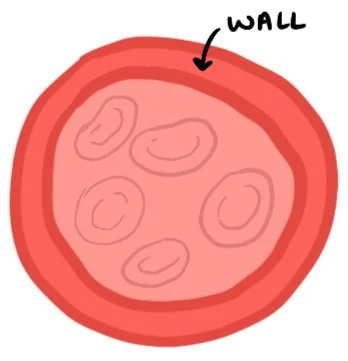
Carbon dioxide is exchanged with oxygen at the level of the alveoli and transported by red blood cells (RBCs).
RBCs circulate throughout the body to targets. Okay, great. Now…
At the cellular level: When you have sufficient oxygen
Sugar (and fat) metabolize through glycolysis in the mitochondria of the cell. Some fancy processes happen to further break down sugar (or fat), producing a lot of ATP (a fancy word for energy). All of this results in very efficient energy production. This is aerobic respiration. There is a long chemical equation that essentially states:
1 molecule of sugar (or fat) + 6 molecules of oxygen = 36 molecules of energy (ATP)*
*It will also produce 6 molecules of carbon dioxide and 6 molecules of carbon dioxide which you’ll exhale, sweat, and pee out.
A normal blood vessel
Insert Exertion and/or Stress
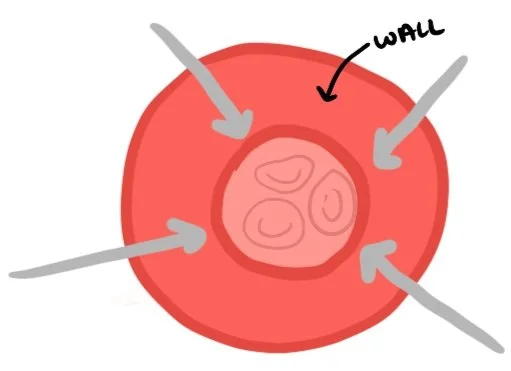
When exertion and/or stress increase, heart rate (HR) increases. As HR increases, the vessels constrict (i.e., vasoconstriction) and blood flow decreases, increasing blood pressure. This can slow (or even impair) oxygen delivery throughout the body (Wirth & Scheibenbogen, 2021).
A vasoconstricted blood vessel
When you have insufficient oxygen…
When there isn’t enough oxygen, the mitochondria skip the fancy processes after glycolysis (the processes that maximize the energy converted) and go straight to fermentation. This overarching respiration process is called anaerobic respiration. This can be fast…but it’s not efficient. Anaerobic respiration produces only 2 ATP whereas aerobic respiration produces 36 ATP for the same sugar+oxygen intake. It also produces a lactic acid byproduct. This lactic acid buildup causes muscle cramps (thus, causing pain) and fatigue (Kelly et al., 2001). This is the body’s safety mechanism for its muscle cells, which, as we can see, can quickly become debilitating for individuals with ME/CFS.
At the cerebral level (when you have insufficient oxygen)…
Cerebral misery perfusion can occur, and it’s just as miserable as it sounds. This causes systemic mayhem:
Fatigue (physical, cognitive, and emotional);
brain fog (“fuzzy” brain);
autonomic dysfunction, including sleep and wakefulness, hunger and thirst, body temperature regulation, and blood pressure;
neuroinflammation; and
cognitive dysfunction, such as attentional deficits, memory and processing difficulties, and challenges with executive dysfunction (Barnden et al., 2019; Daniels et al., 2020; Wirth & Scheibenbogen, 2021).
References
Barnden, L. R., Shan, Z. Y., Staines, D. R., Marshall-Gradisnik, S., Finegan, K., Ireland, T., & Bhuta, S. (2019). Intra brainstem connectivity is impaired in chronic fatigue syndrome. NeuroImage. Clinical, 24, 102045. https://doi.org/10.1016/j.nicl.2019.102045
Daniels, J., Parker, H., & Salkovskis, P. M. (2020). Prevalence and treatment of Chronic Fatigue Syndrome/Myalgic Encephalomyelitis and co-morbid severe health anxiety. International journal of clinical and health psychology : IJCHP, 20(1), 10–19. https://doi.org/10.1016/j.ijchp.2019.11.003
Kelly, D.J., Hughes, N. J., & Poole, R. K. (2001). Chapter 10: Microaerobic Physiology: Aerobic Respiration, Anaerobic Respiration, and Carbon Dioxide Metabolism. In Helicobacter pylori: Physiology and Genetics. ASM Press.
Nguyen, K., D. & Wills, R. A. (2019, September 18). Chronic fatigue syndrome: An autoimmune disorder of the neuroendocrine system. Journal of Biotech Research & Biochemistry, 2(4). https://doi.org/10.24966/BRB-0019/100004
Wirth, K.J., & Scheibenbogen, C. (2021). Pathophysiology of skeletal muscle disturbances in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). Journal of Translational Medicine, 19(162). https://doi.org/10.1186/s12967-021-02833-2